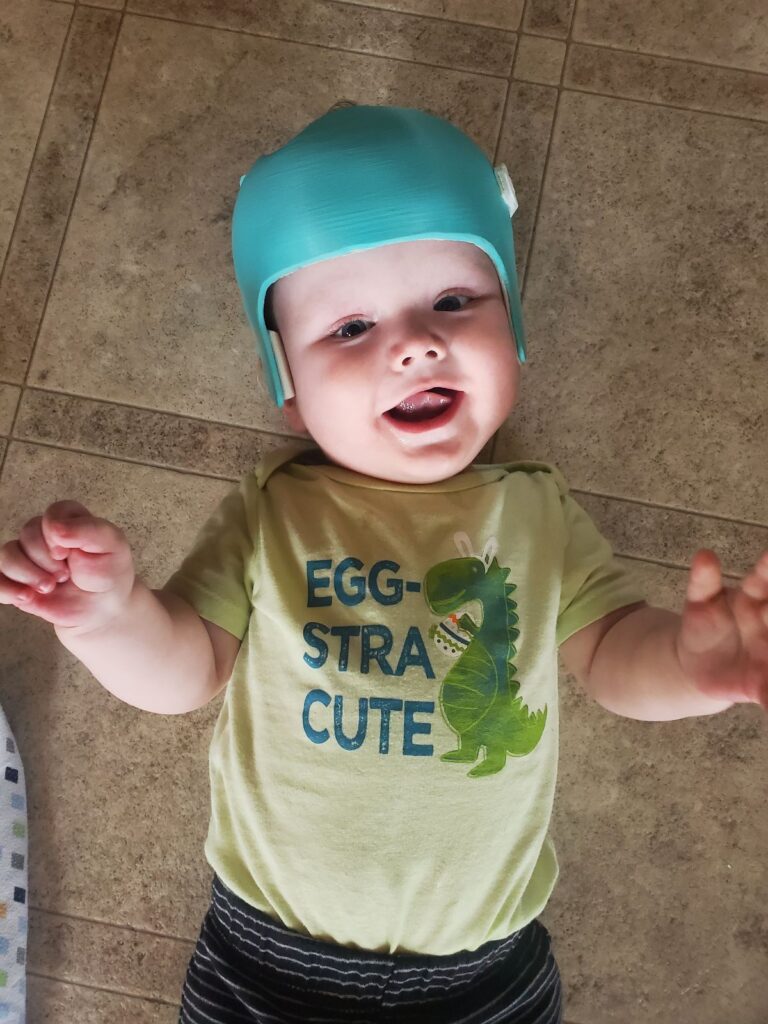
Just in case anyone’s been fruitlessly refreshing this page for the past six months, I thought I’d pop in with an update and a couple of photos from the last month or so.
Last night, Rowan had a seizure which prompted a 911 call and an ambulance ride to Guelph General Hospital. It abated after about an hour, but he continued to have respiratory issues. His medical team has been worried about him aspirating for about a month now (more on that below) and he tested positive for COVID on April 6th, so junk in his lungs is not a surprise at this point. Still, they were worried enough to intubate him and send us for a trip to McMaster’s Pediatric ICU (PICU). Overnight and at a couple of points today he’s had a fever, so it’s obvious that he’s fighting off something. Whether it’s COVID-related, disorder-related, or aspiration-related is mostly inconsequential at this point, and it’s just a matter of getting him better. He’s being treated with some antibiotics, a couple of sedatives to ease his discomfort, and some Tylenol for the fever. It’s mostly just a waiting game, giving his body all the ammunition he needs to get better. While we wait, let me catch you up a bit on the last six months.
Seizures
Rowan’s seizures have been a bit up and down the last six months. Throughout November and December we were in hospital every other week with seizures, including a two-night stay at McMaster over Christmas. January was fairly quiet with mostly ones we were able to control from home, but then February roared back with a vengeance with three 60+ minute seizures that sent us down to McMaster each time. March only saw one short ~2 min seizure that didn’t even require a dose of rescue medications, and last night’s was the first we’ve had in April.
While there doesn’t seem to be a lot of rhyme or reason to the length or severity of the seizures, they almost always occur between 6pm and 9pm. Some of the seizures seem to be attributable to other stresses put on his body – an illness, a vaccination, or some outside circumstance that brings about a seizure. Others don’t seem to have a specific cause.
In general it feels like we’re honing in on a good approach with his medication. We’re getting great advice from other families in the TESS community for the types of anti-seizure medications that seem to work well for kids with SLC13A5 disorder. Now that Rowan’s not growing quite as quickly we can get into a more consistent routine in terms of dosage. Since February he’s been taking five anti-seizure medications twice per day orally, with the plan being to wean him from one of them if his seizure activity drops. No word yet on how last night’s episode will play into that.
Physiotherapy
Rowan’s been having regular physiotherapy, both at home and a clinic in Waterloo, to help him grow stronger and hit his milestones. At home we do regular exercises with him to improve his muscle tone, though he’s been slowed down the last two weeks because of COVID. He’s getting a lot closer to rolling from his back to his front, and his neck support has significantly improved over the last couple of months. It’s slow going but he’s getting there. Progress is progress.
Feeding
Rowan participated in a swallowing study through McMaster in March to determine how well he’s been eating. His low muscle tone impacts all of his muscle systems, including those in his neck involved in swallowing. They found that food, both solid food and formula, has been finding it’s way into his airway and is causing some breathing issues. Sometimes he’ll cough it out, other times the food will just… sit there, and afterwards he will keep smiling even as he’s wheezing away. Not ideal. His medical team is worried that this could lead to possible lung infections in the future (or already has… see above), and that his body is expending a lot of energy just constantly healing his respiratory system—energy that could be better used on improving muscle tone in other parts of his body.
The recommendation is to insert a G-tube, a small surgery that places a tube through his belly and allows us to deliver nutrition directly to the stomach. This is likely to occur fairly quickly, but not until he’s at least a little bit better. Likely in the next three or four weeks. We’ll continue to work to improve his mouth and swallowing muscles using things like thickened formulas to get to a point where he can eat regularly, but in the meantime the G-tube will make it easier not just to ensure he’s getting all of the nutrients he needs, but also to easily administer all of those meds.
Lightning Round: Other Updates
- We’ve been referred to SickKids to meet with their respiratory medicine team on all of the breathing stuff (and some other stuff I didn’t get into)
- Rowan has a couple of teeth coming in! We’ve also been referred to SickKids for those as well, as SLC13A5 can cause abnormalities in tooth enamel. Just trying get on top of things early and hopefully stay on top of them.
- As of April 1st, Amber’s back to working remotely for Skyline and I’m on parental leave until the end of May. All three of us seem to adapting pretty well to the change.
- Rowan’s been dealing with reflux, and is on a couple of medications to help address that.
- His adenoids are slightly large which is one of the reasons he is so “snorty”. He’s got a steroid spray that seems to have helped a lot in the last month.
- Rowan has a positive prescription in his left eye. Further testing is forthcoming to determine what he may need to address that.
- A promising gene therapy for SLC13A5 is in development, and trials will likely begin in the next six-months or so. We’re hoping to be a part of those trials.
- The team at TESS continue to be an incredible resource for us. If you have some money burning a hole in your pocket, I can personally vouch for the work they do and you can be sure your every cent will be put toward research and treatments for this disorder.








